The evolution of omega-3s: From heart to brain health

Groundbreaking heart health studies in the 20th century now serve as a springboard for a myriad of research into other health conditions, including dementia. The question is not whether omega-3s can promote brain health, it is what new studies scientists can create to further substantiate the evidence.
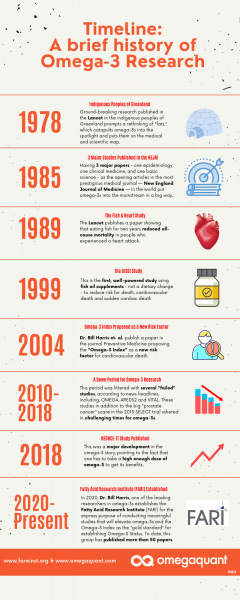
As researchers continue the exploration into omega-3s, NutraIngredients-USA looks back at the seminal research that propelled the nutrient onto the health stage and what is to come in the decades ahead.
Cardiovascular health among the Greenlandic Inuit
The use of omega-3s as a supplement dates back to at least the late 1700s when British doctors used cod liver oil to orally treat the symptoms of rheumatism.
“When the patients stopped using cod liver oil, the symptoms returned,” said Sam Wiley, founder and managing partner of supplement consulting firm Skysail Solutions. “So that’s when doctors wrote up [their findings] as a case study.”
Despite efforts at early research, scientists understood the effectiveness of fish oil only through anecdotal or observational evidence.
That changed centuries later when in the 1970s Danish researchers led by Jørn Dyerberg and H.O. Bang compared the diets and cardiovascular health of the Indigenous people of Greenland to the population of Denmark.
The researchers found that the Greenlandic Inuit had lower risk for primarily acute myocardial heart attack than Danish citizens on the mainland. At the time, the Inuit consumed 16,000 milligrams per day of EPA and DHA, dietary fats that comprise omega-3s.
“There's this fat paradox,” Wiley said. “You should have lots of heart attacks and cancer with a high fat diet. But the Greenlandic Inuit eat this really high fat diet, and they don't have heart disease.”
The researchers examined cholesterol levels, triglyceride levels and blood pressure, among other measures. Then they analyzed the Inuit’s food as well as their blood levels for EPA and DHA and compared that to the food and blood of people living in Denmark. The researchers tested the effects of DHA in food and blood on platelets, platelet function and platelet aggregation to test blood clotting.
They found that EPA was highly effective at preventing platelets from sticking together, thwarting heart attacks caused by an acute blood clot in the coronary artery.
The researcher’s findings were published in 1978 in The Lancet. They proposed that EPA in the Inuit diet was antithrombotic, which explained the decreased risk of heart attack.
Twentieth century gains, 21st century stumbles
The late 20th century marked a heyday for omega-3 research into cardiovascular health. By 1985, the New England Journal of Medicine had published three landmark studies—one epidemiological, one clinical and one basic science—espousing the benefits of omega-3s. Among the findings, researchers suggested there was an inverse relationship between fish consumption and 20-year mortality from coronary heart disease.
In 1989, scientists published results from the DART Trial, which noted that giving patients who suffered a heart attack oily fish for two years reduced all-cause mortality by 29%. By 1999, the biggest omega-3 “bombshell study of all” was published, according to OmegaQuant, the company behind the Omega-3 Index, a test that evaluates omega-3 status.
“[The GISSI-Prevenzione trial] was important because it was the first, well-powered endpoint study to use fish oil supplements—not a dietary change—to reduce risk for death, cardiovascular death and sudden cardiac death, all without meaningful lowering of cholesterol or triglycerides,” OmegaQuant said.
However, that success was followed by a down period for omega-3s.
“The years between 2010 and 2018 were not happy times for omega-3s,” OmegaQuant added. “This nearly 10-year drought was littered with several ‘failed’ studies: OMEGA, ORIGIN, Risk and Prevention, AREDS2, VITAL and ASCEND.”
Additionally, the big prostate cancer scare in the 2013 SELECT trial suggested that fatty acids were involved in prostate tumorigenesis.
By 2018, more research espousing the benefits of omega-3s began to surface. In the REDUCE-IT trial, participants were given 4 g/day of EPA, which reduced cardiovascular disease by 25% in patients on statins. This was followed by the STRENGTH trial that studied effects in a similar population with 4 g of EPA+DHA.
The brain research
Although the 20th century brought notable research insights regarding omega-3s and cardiovascular health, the 21st century is proving just as compelling due to the potential of the fatty acids in other areas, such as in eye health, inflammation and, maybe most notably, the brain.
“If you look at a lot of small trials that have been conducted on omega-3s, there's been evidence that shows that if you get a high dose, then you start to see some cognitive impacts, improvements,” said Adam Ismail, chief strategy officer at the KD Pharma Group, an omega-3 manufacturer. “I think there's a need to be confirmed in larger trials.”
Whereas cardiovascular disease is a relatively easy area to conduct trials because there are well accepted biomarkers for things like cholesterol and blood pressure, he said, "Alzheimer's is a difficult thing to measure because there aren't biomarkers for it that are validated and accepted."
There’s also the concern of who will pay for the large-scale studies to determine the impact of omega-3s on dementia. Nutraceutical companies have not funded much omega-3 research, and if they have, it's been with in vitro or animal studies, Ismail added. The work has been largely funded by academic and government grants, even more so than the pharmaceutical industry.
In 1948, researchers began the Framingham Heart Study, a long-term, multigenerational analysis of the characteristics that contribute to cardiovascular disease. More than 14,000 people have participated in the study. Beyond heart health, scientists are examining other parts of the body and how it responds to diet, including omega-3s.
“[With Framingham], we reported a significant inverse relationship,” Bill Harris, president and founder at both Fatty Acid Research Institute (FARI) and OmegaQuant. “A higher omega-3 index lowers risk for cardiovascular disease and for total mortality in Framingham.”
The inverse relationship also exists with dementia.
“We looked over the next seven or eight years who developed dementia, and you find out the people who had the highest omega-3 levels were like 50% less likely to develop dementia,” Harris explained. “If we could really get people to have high omega-3s in their 20s, 30s, 40s, it's going to postpone the time they actually become disabled.”
In the meantime, he said that if people increase DHA levels in the brain, it will reduce the risk of not only Alzheimer’s, but bipolar disorder and depression, among other ailments. Understanding those connections comes from the groundwork laid by decades of earlier research into omega-3s impact on the body.
“You keep doing additional studies and you keep asking additional questions to begin studying mechanisms of action,” Harris added. “When it comes to omega-3s, nothing surprises me anymore.”